Do you dread taking the first few steps of a morning?
Can’t handle standing on your foot for too long?
Do you experience pain in your arch or heel?
If you answered YES to these questions you may in fact be suffering from a condition called Plantar Fasciitis. You are probably thinking plantar what??? And how on earth do I get rid of this darn thing! I bet you have tried resting and changing shoes and you may have found some temporary relief with this but I bet it hasn’t disappeared. Sounding familiar?
Let’s start with what exactly is the plantar fascia?
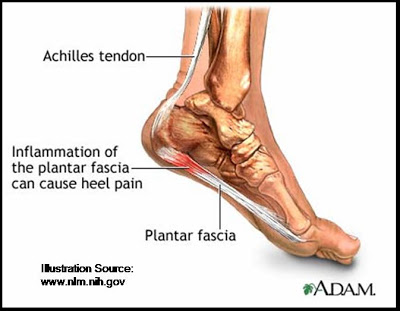
The plantar fascia is a normal structure in the foot and it runs from the base of the heel bone (calcaneus) all the way up to the longer bones of the foot. The plantar fascia is not a muscle but rather a piece of fibrous tissue that functions to support the arch of the foot, binds the sole of the foot upwards and protects the sole from injuries. If you think about it this way, imagine walking on the same tissue that’s on the inside of your thigh, its not going to function very well. Hence the fascia is what provides the tautness and elevation to the tissue on the sole of the foot.

How would I know if I had plantar fasciitis?
First of all, it is always best to see a qualified physiotherapist who can correctly diagnose you however some of the common symptoms you may be experiencing include;
- Pain upon first rising in the heel
- Pain in the heel that feels like a stone bruise to walk on or touch
- Pain may be present when you start activity, settle once you are warmed up and then return with rest
- Reduced ability to stand for prolonged periods due to pain in the heel
Why have I got this condition?
- Age
Plantar Fasciitis is almost exclusively seen in the adult population and increases in prevalence between the ages of 40 and 70. However this is not to say people in their late teens and early 20’s can’t develop it as I have definitely seen severe cases in these groups too.
- Obesity/Weight Gain
Carrying excess body weight or rapidly gaining weight adds considerable load onto the plantar fascia. This can be enough to cause an overload and thus pain.
- Biomechanical Factors
These are largely out of your control however increased pronation (commonly termed overpronation) causes increased stress on the fascia and its insertion. On the contrary, a very high arch (pes cavus) has also been associated with this condition. Additionally, tightness of the muscles in and around the foot may also contribute to overloading the plantar fascia.
- Changes in activity
A sudden change in activity, especially those that involve increased weight bearing is strongly correlated to the development of this condition. This could be a seemingly small change such as going from sedentary and working at a desk to walking 3 times per week for 20 minutes. On the opposite end of the scale going from running 3 times per week to running 4-5 times per week could also incite the condition.
- Footwear
Poorly fitting footwear or shoes that do not have adequate arch support for your foot type may predispose you to the development of this condition. While many brands such as Nike, Adidas and Under Armour (to name a few) are more fashionable they often lack the medial arch support and cushioning required to maintain optimal foot health. Additionally, a sudden change in footwear (to a less supportive shoe) can also trigger pain.
Did you notice a pattern from the above?
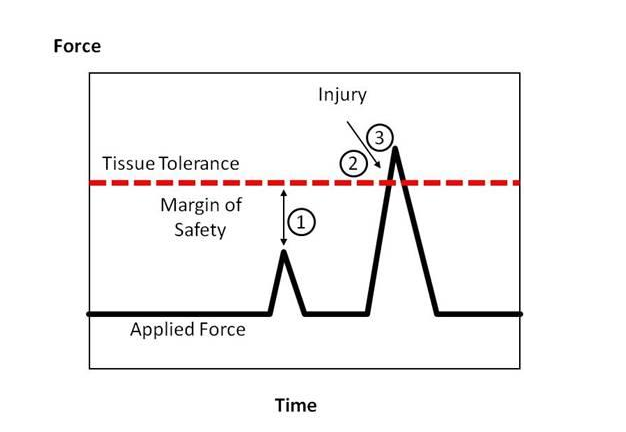
Plantar fasciitis is all about LOAD!!!
Changes in LOAD can be changes in frequency, intensity, duration, weight or type of activity. You are far more likely to get a plantar fasciitis if you go from a gym based program to walking/running than the other way around. This is because of the repetitiveness and weight bearing component with this type of exercise.
OK so perhaps you’ve had the ahuh moment and may have figured out what triggered this condition to start.
So the question everyone wants to know is how do I get rid of this??
Firstly, get an assessment done by a qualified physio who will then put you together a treatment plan, estimated rehab/recovery time frame and can guide you on the do’s and don’ts to enhance your recovery.
Assessment will firstly confirm the diagnosis through listening to your history, aggravating and easing activities as well as confirming the pain source/location. From here we will determine your load tolerance, that is how much can you do right versus left leg in terms of calf raises, hopping etc (depends on how sore you are).
Treatment:
Treatment can be broken down into active or passive treatment interventions. Both have their place but perform different roles in your recovery. I strongly believe that BOTH are essential for a full recovery.
- Active
Active interventions are the biggest part of treatment and are what will get you back to your desired activities. They include specifically prescribed exercises that are customised to YOU, your functional level and noted deficits. We are able to determine your functional level from your load tolerance test listed above. The exercises prescribed are designed at strengthening the calf and increasing the load tolerance of the plantar fascia. A typical exercise would be a single leg calf raise with the big toe elevated (in dorsiflexion if we are talking physio terms). However, depending on your level of soreness will depend on where we start.
We may also include some exercises for the smaller muscles of the foot that commonly don’t function optimally in people with this condition.
- Passive
Passive interventions include things such as massage, acupuncture, ice/heat. Passive interventions are designed at pain relief in the short term but will not assist with improving the load tolerance of the fascia. Some of our best passive interventions we use include;
- Ice water bottle massage – freeze a cylindrical shaped water bottle and after activity roll the arch of your foot on the bottle for about 5 minutes.
- Golf ball massage – for a deeper massage you can try rolling the arch of the foot on a golf ball with as much pressure as is comfortable. Avoid getting stuck in to the heel where the fascia inserts as this tends to make things more painful.
- Stretches – Stretching the calf muscles may assist with reducing feelings of tightness in the calf and plantar fascia. If your pain is bad enough you may have started to limp which can cause surrounding muscles to become tight.


Frequently Asked Questions
What about Orthotics?
Firstly, not everyone requires orthotics who has plantar fasciitis. If we feel you have a particularly low arch that is contributing significantly to your pain then a podiatry review for potential orthoses is warranted. However, remember our load talk above…if you have been wearing thongs instead of runners on holidays for 6 weeks and have developed this condition orthoses may not be the answer for you. Similarly, if you have suddenly changed activities and the pain has come on trialling conservative, exercise-based rehabilitation first should be the first line of treatment. Should you fail to see a change or we don’t get the 100% full return to function desired then orthoses may be of assistance. Our physiotherapists would usually refer patients to a podiatrist to have a pair of custom orthoses made opposed to using prefabricated ones. This is to ensure a comfortable fit that will offload the plantar fascia specific to that person.
My friend had a cortisone or steroid injection and they said it made the pain go away, should I just go and get one of those?
Again, remember what we said about load…plantar fasciitis comes about because your load exceeds the fascia’s ability to recover. Yes, a steroid may assist in your pain but it will do nothing for improving your load tolerance. Therefore, when the steroid loses its effect (anywhere up to 6 months) there is a high probability of the pain returning. Additionally, research has shown the steroid can have a negative effect on tendons and the fascia over the long term resulting in a weakening of the tissue (the opposite of what we are trying to achieve!!). Our recommendation is always to trial conservative exercise based treatment first as this has been shown to be most effective in long term management and return to activity.
How long will this take to resolve?
The duration of the condition depends on how long you have had symptoms prior to seeking treatment, adherence to a specific exercise program, adherence to recommendations regarding loading/offloading and footwear and individual factors. Individual factors which may delay recovery include conditions such as diabetes which have been associated with slower healing rates. In some people they will be significantly better after 6 -12 weeks of treatment and in more severe cases it can be up to 2 years.
If you or someone you know is suffering from heel or arch pain encourage them to see a physiotherapist. This can be a debilitating condition but with the right treatment the pain can be reduced and function restored. If you would like to book an appointment to see one of our friendly staff please call our clinic on 9672 6752 (Kellyville) or 9871 2022 (Carlingford).
Kimberley Cochrane (Bach Physiotherapy, First Class Hons; Grad Cert Sports Phys)

