Have you ever woken up with pain or pins and needles in your arms or legs? It’s called radiculopathy and unfortunately it is not as uncommon as you think! About 100 women and 60 men per 100 000 will experience radiculopathy and it is most common in people who are aged between 40 and 50.

What is radiculopathy?
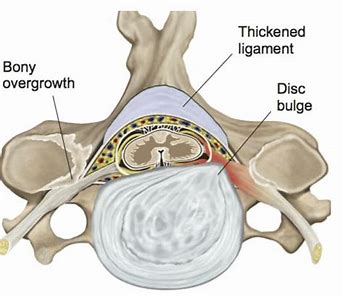
Radiculopathy describes most kinds of nerve root dysfunction, either because a nerve is being directly irritated at the spine itself or because of inflammatory chemicals which can be released by injured discs. The most common source of irritation tends to be direct mechanical compression, mostly due to spondylosis. Spondylosis refers to degenerative changes which occur due to advancing age. As we get older, the discs lose height and the canals through which our nerves exit from our spine begin to narrow. These changes lead to increased load on the vertebral bodies and joints within the spine, causing bony changes and thus irritation of the nerves. Nerves can also be irritated by herniated disc contents, although this is less common. Radiculopathy due to disc herniation tends to present more in younger people, whilst spondylosis is a more prevalent presentation in older populations.
Radiculopathy usually presents with pain and/or altered sensation running down the arm or leg. Altered sensation can include pins and needles, numbness, burning or tingling. Other symptoms include muscle weakness in the affected limb and reduced reflexes. Radiculopathy is mostly a self-limiting condition and about 75-90% of people get symptomatic relief with conservative physiotherapy treatment. In the absence of significant muscle weakness or myelopathy (injury to the spinal cord due to severe compression), physiotherapy is a clinically indicated treatment modality.
How can physiotherapy help?
Most literature has come to a consensus that manual therapy in conjunction with therapeutic exercise is effective in dealing with radiculopathies. Physiotherapy treatment would normally comprise of a combination of manual therapy, intermittent traction (where the therapist would stretch from either the head or legs to decompress the spine and reduce nerve root irritation) and exercise. It is important to note that exercise is the most sustainably beneficial treatment method for radiculopathy. Manual therapy alone usually does not provide clinically significant relief when used in isolation. It is usually the combination of manual therapy and exercise which provides the best long-term results.
Early-stage therapeutic exercise will primarily consist of restoring pain free range of motion, usually by working through active range in the opposite direction. Once range of motion has been restored, strengthening exercises will also help provide stability and active support for the spine, reducing the risk of recurrence. Early strengthening will primarily consist of isometric strengthening until peripheral symptoms resolve. This will transition to progressive strengthening through range, and incorporation of shoulder stability work in the case of cervical radiculopathies or core strengthening work in the case of lumbar radiculopathies.

Shoulder stability is clinically significant due to its implications for our neck as we have a lot of musculature which crosses over the neck and the shoulder. Therefore, we often find that when our shoulder is weak it can lead to an associated neck issue and vice versa. Examples of shoulder stability exercises include scapular retraction based work and closed chain exercises to improve weakness of shoulder girdle stabilisers. This is supplemented by localised deep neck flexor strengthening with particular emphasis on fine motor control, and activation of deeper musculature without excessive compensation by superficial muscles. With lumbar radiculopathies a progressive core strengthening program that focuses on activation of both transverse abdominus and multifidus muscles has been shown to improve radiculopathies.
Prognosis:
Radiculopathy in the absence of severe muscular weakness, spinal cord damage or progressive neurological signs can be treated with physiotherapy and usually has a good prognosis. Factors which are predictive of a good recovery include:
- Age under 54
- Dominant limb not affected
- Looking down does not aggravate symptoms
- Treatment involving a combination of manual therapy and good compliance to exercise interventions
Remember, manual therapy is helpful but it is even more effective when supplemented with a specific exercise program targeted towards your needs.
If you have pain or abnormal sensation in your arms or legs which isn’t correlated to a direct injury, our physiotherapists will be able to assess your condition and provide a tailored treatment plan for you. Please get in touch with us on 9672 6752 (Kellyville) or 9871 2022 (Carlingford) and one of our friendly receptionists will be able to arrange an appointment for you.