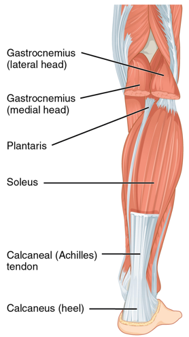
The muscles at the back of the lower leg are commonly referred to as the calf muscles. They begin at the back of the knee and travel down and insert at the back of the heel. They are essential muscles in walking, running or jumping.

There are 3 muscles which make up the calf. These three muscles combine to make up the tricep surae:
- Gastrocnemius – this is the most superficial muscle of the calf and has two heads: medial (inside) and lateral (outside). These two heads form one single larger muscle. This muscle helps in plantarflexion (pointing your toes) and flexing or bending the knee.
- Soleus – this is a large flat muscle located underneath the gastrocnemius. This muscle starts below the knee so has no function at the knee. It joins with the gastrocnemius to form the calcaneal tendon and inserts into the back of the heel. It is a powerful muscle which is important in walking, running and keeping balance.
- Plantaris – this is a thin, small muscle which has the same actions as the gastrocnemius. About 10% of the population don’t actually have one.
These muscles join and form the calcaneal tendon, commonly known as the Achilles tendon. This tendon is the largest and strongest tendon in the body, however, is subject to injury. Calf injuries are common particularly in ball sports where there is a need for sudden acceleration.
Muscle injuries: the medial head of the gastrocnemius is the most common site of a calf injury.
- Calf strain: tearing of a portion of the muscle fibres commonly referred to as a pulled muscle, it can vary in severity. Rehabilitation will consist of range of motion exercises, gentle stretching and progressive strengthening exercises.
- Calf rupture: this is a complete tear of the calf muscle. This can lead to extreme pain and being unable to stand or walk on the leg. Treatment of this may differ depending on severity and can be managed conservatively or surgically.
Tendon injuries:
- Tendinopathy: This is the most common Achilles injury and is caused by an overuse injury of the tendon. A tendinopathy can occur either in the middle of the Achilles tendon or where it attaches to the heel (Insertional Achilles tendinopathy). It can lead to pain and stiffness in the tendon especially of a morning and pain at the start of activity. Exercise is a vital aspect of rehabilitation and will incorporate both strength and endurance training.
- Achilles tear: this involves a tearing of a portion of the tendon fibres. This can lead to pain and a decrease in function of the calf muscles.
- Achilles rupture: this is a complete tear of the Achilles tendon which will result in an inability to plantarflex your foot. At the time of the injury you may hear an audible “pop” followed by some swelling and pain. A common descriptor is it felt “as if I was hit or kicked in the back of the leg”. Males are more likely to experience this and usually occurs in athletes in their 30’s and 40’s. This will generally require a specialist opinion. Rehabilitation will involve a camboot, gentle range of motion exercises and a strengthening program once the camboot is removed.
- Bursitis: inflammation of a fluid filled sac that sits underneath the Achilles tendon. The bursa allows the tendon to move easily over the bone. When inflamed it can cause pain and tenderness around the heel area. Bursitis is often found in conjunction with an insertional tendinopathy as the inflammation and tendon compress the bursa resulting in irritation of the bursa.
- Sever’s disease: this is inflammation of the growth plate in the heel where the Achilles tendon attaches. It is common in adolescents experiencing growth spurts as bones, muscles and tendons are all changing rapidly. Repetitive stress from running and jumping can inflame this area and therefore children in athletics are at an increased risk. Physiotherapy treatment is likely to involve stretching of the Achilles tendon to reduce the stress on the heel and a strengthening program.

Not to be missed:
- DVT (deep vein thrombosis): this is a blood clot in a deep vein in the body, usually in the calf. Symptoms of a DVT are tenderness in the calf usually described as a cramping feeling, reddish or bluish skin and skin around the calf warm to touch and pain in the calf area. If you are experiencing these symptoms you should call for medical help or go to the emergency room where they will be able to test for DVT.
Brooke Sullivan (Bach Ex Sci Sports Mgt; Masters Phys)

